Frequently Asked Questions
Patients
If I’m receiving hospice services, do I have to stay home all the time?
Can I take myself off hospice?
If I come off hospice, can I re-enroll later?
I want to enroll in hospice – what happens next?
If I’m receiving hospice and need to move, will the same hospice care team still care for me?
What do I do with the medications I’m currently taking when I go into hospice?
What makes Kaiser Permanente hospice unique?
As a Kaiser Permanente member, you’ll receive high-quality care while in hospice, just as you do in our medical facilities. Patients with complex conditions choose Kaiser Permanente for their hospice needs because of the continuity of service, high-quality medical care, and caregiver support. Our comprehensive electronic health record contains your medical information, which can be accessed by your Kaiser Permanente providers.
Where are hospice services provided?
Hospice is provided anywhere you call home. This includes a house, an apartment, co-op, a skilled nursing facility, board and care residence, assisted living facility, or even a friend’s or relative’s home. In some circumstances, if a hospitalization is needed for comfort, hospice can also support you during this time.
Do people on hospice die sooner than people not on hospice?
No. In fact, research shows that the high-quality care and support given hospice patients more often leads to a longer lifespan. 1
While it’s true that people who are on hospice have chosen to no longer focus on curative treatments, it does not mean they’ll die sooner. It’s essential to talk with your doctor and loved ones about what decision is best for you.
Can I call 911 for an emergency?
If you have an emergency, start by contacting your local Kaiser Permanente hospice care team first. The hospice nurse and doctor may be able to ensure your safety and comfort through an emergency situation while avoiding the stress of an Emergency Department visit.
In certain instances, 911 services may be a useful tool when used in coordination with the hospice care team. Ask the hospice care team for more information about this.
What is a comfort care medication kit?
The hospice care team will provide you with a comfort care medication kit to keep at home so symptoms can be managed in a timely manner. This kit contains small amounts of different medicines to treat symptoms that may occur toward the end of life.
Information about dosage, instructions for administering, and the symptoms they treat can be found both here and in the hospice binder, although call Hospice before using any of the medications.
Read more
Hospice Comfort Care Medication Kit and Usage Instructions
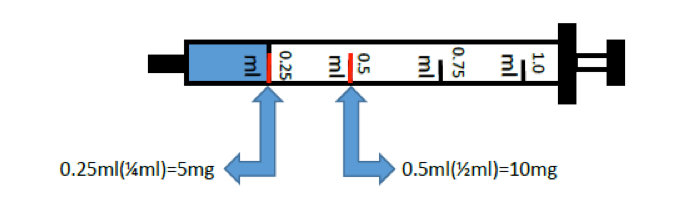
A one-millimeter syringe
| Medication | What It’s For | How to Take |
|---|---|---|
| Morphine oral solution (see image above) |
A concentrated liquid medication used for pain and/or shortness of breath. Concentrated so only a small dosage is needed. A one-milliliter syringe (1.0 ml) without a needle (see image above) is included. | Can be swallowed or given under the tongue.
If swallowed, can be diluted in a small amount of fluid (water or juice) or given in soft food (pudding or applesauce) |
| Ativan tablet | Commonly used for anxiety, agitation, insomnia, seizures, and shortness of breath | May be swallowed or given under the tongue |
| Haldol oral solution | Commonly used for nausea, vomiting, and/or agitation | May be swallowed or given under the tongue |
| Atropine solution | Commonly used for increased secretions
Note: Do not give in eye |
Given under the tongue |
| Phenobarbital tablets | Commonly used for agitation and/or seizures | May be swallowed or given rectally |
| Bisacodyl suppository | Commonly used for constipation | Given rectally |
| Acetaminophen suppository | Commonly used for fever and/or mild pain | Given rectally |
| Lubricant | For ease of use for rectal administration of medications | For rectal use |
Please do not use any medication in the comfort care medication kit until instructed to do so by your hospice team. If you have any questions regarding the comfort care medication kit, call your hospice care team.
Your hospice nurse will check your comfort care medication kit regularly for expiration dates and to make sure you have the correct medications with the correct quantity.
Read less
How to dispose of needles and syringes (‘Sharps’)
California state law requires that all needles and syringes, which are shortened to medical ‘Sharps’, must be disposed of properly and NOT thrown out in regular household trash.
To find the nearest Sharps Waste Disposal collection site in your area:
Call 1-800-CLEANUP, choose the option for Medical Sharps, then enter your zip code
or
Visit www.safeneedledisposal.org
DO NOT put sharp objects in any container that will be recycled or returned to a store.
DO NOT use glass or clear plastic containers to dispose of Sharps.
DO NOT keep containers with sharp objects within reach of young children.
If I’m receiving hospice services, do I have to stay home all the time?
No, you don’t have to stay in your home. If you’re physically able and interested in going out, you may leave your home. Going outside for a few minutes or for a day trip is up to you. It’s based on what you want to do, as well as what you are physically able to do.
Can I take myself off hospice?
Yes, you may choose to discontinue hospice for any reason at any time. If your life expectancy improves or you decide to seek life-prolonging or curative treatments, your hospice care would be discontinued.
If I come off hospice, can I re-enroll later?
Yes, if you decide later that you are interested in receiving hospice services again, you can reapply.
I want to enroll in hospice – what happens next?
The first step is for your doctor to refer you to the hospice department.
A hospice nurse will call to talk to you about the hospice program and determine if you qualify. If you do, another hospice nurse or a medical social worker will visit you at your home to ask additional questions, explain more about the hospice program, review your current medications, and have you fill-out and sign the hospice consent form. You may receive a follow-up phone call to see how you are doing and give you a chance to ask questions.
Read more
You’ll receive a packet of detailed written information about Kaiser Permanente hospice.
The hospice nurse in charge of your care, sometimes called your case manager, will visit your home to meet you and discuss your medical needs as well as your non-medical needs, such as support from a social worker, spiritual counselor, or volunteers.
Depending on your needs and what works best for you and your family, other members of the care team will visit your home as well. Although your hospice doctor won’t routinely visit your home, they work closely with the hospice nurse and other care team members to coordinate your care.
If you need to speak with Kaiser Permanente hospice care team staff, call the Hospice department 24 hours a day, 7 days a week.
Read less
Can I still go to my primary care or specialist doctor, like my cardiologist or oncologist, for care if I’m on hospice?
The goal of hospice care is to provide a comfortable life, away from the inconvenience or discomfort of excessive or unhelpful medical treatments. The hospice care team, often working together with your other doctors, can manage your care without the need for regular doctor visits. However, there are some circumstances where a visit to your doctor may be helpful and appropriate.
If I’m receiving hospice and need to move, will the same hospice care team still care for me?
If you move within 15 miles or 30 minutes of a Kaiser Permanente service area, you will still be cared for by Kaiser Permanente hospice, although you will probably have a new hospice care team.
If you move more than 15 miles or 30 minutes outside of a Kaiser Permanente service area, you will be referred to a non-Kaiser Permanente hospice service. You will still have a doctor, nurse, social worker, spiritual counselor, and other providers who will be familiar with your health and circumstances.
What do I do with the medications I’m currently taking when I go into hospice?
When you begin hospice, your hospice doctor will create a new medication plan for your medical needs. The focus will be on comfort and treatment of symptoms, like pain, shortness of breath, or anxiety, so some of your medications may no longer be recommended or needed.The hospice care team can tell you what to do with those medications, which may include stopping them, as well as provide instructions on your new medications.
- Source: nhpc.org/press-room