Help with Symptoms
We recommend reading this section in advance so you can easily find the information when you need it.
Agitation
Many patients who are in the last weeks or month of life may become agitated, restless, or confused. An agitated person may show swift changes in mood or behave differently than normal. Sometimes, they may even hallucinate, seeing or hearing things that aren’t there. Agitation can be caused by changes in the body during the last stages of life. It can also be caused by physical discomfort, such as pain or the need to empty the bowels or bladder. Depending on the cause and severity of a person’s agitation, there are different options to help alleviate it.
Read more
First, call the hospice care team to
- Assess the distress to determine its cause
- Provide medications if appropriate
- Provide pain medications if needed
Ways caregivers can help
- Avoid startling the patient, such as not abruptly waking them or turning on bright lights
- Identify yourself with a warm greeting in case they’ve forgotten who you are or don’t recognize you
- Create a calm environment, like playing soothing music or speaking quietly
- Offer emotional support to a patient who may be dealing with unresolved life issues
Read less
Anxiety
A patient with a serious illness can be anxious, with anxiety ranging from mild to severe, as well as day-to-day. To support and comfort them, remind them of the importance and impact their life has made, and soothe and remind them that their responsibilities are being handled. If caregivers need specific strategies or support to help manage a patient’s anxiety, the hospice care team can help.
Read more
- The hospice nurse can help with physical symptoms that may be causing anxiety, like pain and shortness of breath. The nurse can also help explain to the patient about their illness and its progression, to help prevent fear and worry of the unknown.
- The hospice medical social worker or spiritual counselor can talk with the patient about unresolved issues or uncertainties around death and what will happen after they pass away.
- The hospice care team can help caregivers manage the ups and downs of the dying process.
Read less
Bedsores
Bedsores, also called pressure ulcers, are injuries to the skin that happen when pressure is applied, like lying in bed for long periods of time. Body parts in contact with a bed or seat are at risk for bedsores.
Read more
Often starting out as redness or tenderness on the skin, bedsores can become a blister, sore, or open wound as they get worse. While the best way to handle bedsores is to prevent them from happening, bedsores may still appear even with good care. The hospice care team can show you important steps to help prevent or lessen bedsores.
What a patient can do
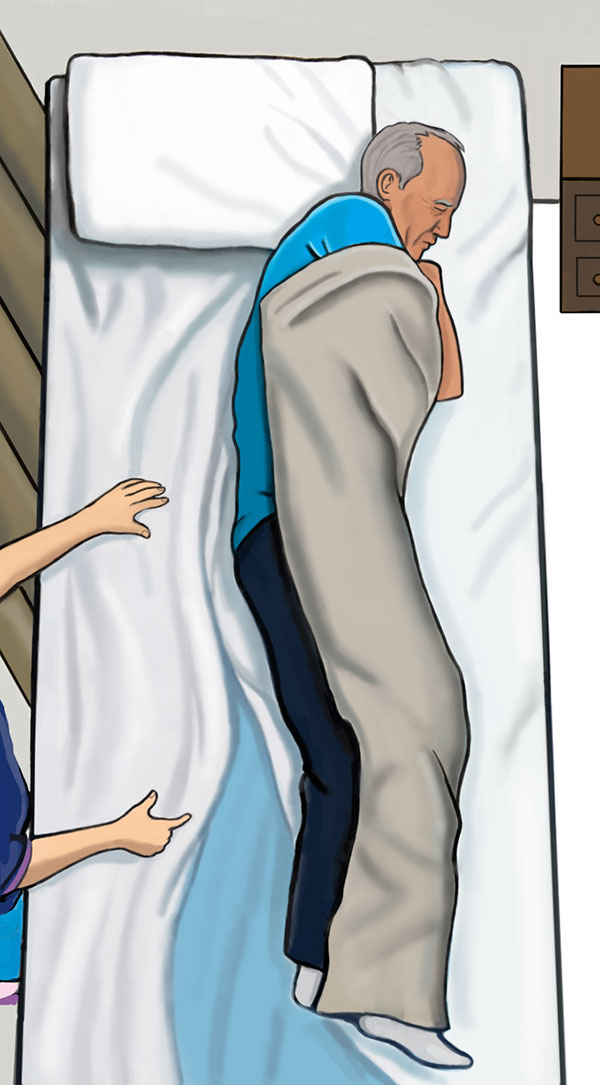
- Reposition throughout the day. The more a position is changed, the better. Try moving every 15 minutes if possible. A patient in a wheelchair or chair can lift with their arms until their back and bottom lift off the cushions. For a patient in a bed, turning or repositioning so a different part of the body touches the bed.
- Keep skin clean and dry. Use gentle techniques, such as sponge baths or patting dry the skin instead of scrubbing or roughly drying the skin. Putting lotion on very dry skin or talcum powder on hard-to-keep-dry areas can also help.
- Protect bony areas. Place extra cushioning on areas that receive a lot of pressure, like the tailbone or shoulder blades. In bed, try to avoid sleeping directly on the hips. Instead, sleep slightly tilted to the front or back and use pillows to prop up the body. Place cushions between the knees and ankles to keep them from pressing into one another. Place a cushion under the calves to keep heels from touching the bed.
What a caregiver can do
- Regularly change bedding and clothing. If the patient wets the bed or has a bowel movement, try using diapers or a disposable pad underneath. Changing bedding, disposable pads, and diapers regularly helps prevent conditions that may lead to bedsores.
- Move and reposition a patient when they can no longer do it themselves, ideally at least every 2 hours, though more frequently is fine.
- Check the patient’s skin on their entire body for signs of emerging bedsores. Check daily. Your hospice care team can help check when they visit.
- If there are signs of a bed sore, try to keep the area from pressing against any surfaces and alert the hospice care team who can help treat the area.
What the hospice care team can do
- Help the patient treat a bedsore by keeping it clean and helping minimize further damage.
- Show the caregiver how to reposition the patient without hurting themselves, using safe lifting techniques or a towel or sheet underneath the patient to shift them. The hospice care team can also help with repositioning when they are visiting.
As always, contact the hospice care team if you need any support.
Read less
Changing Bedsheets for Immobile Patient
If the patient is able, have them get up from the bed while you change the sheets.
Read more
If the patient is unable to get up from the bed to change the sheets, you will have to make the bed one half at a time. Here’s how to do it.
- Remove pillows and any sheets that are on top of the patient.
- Have the patient bend both their knees.
- Have the patient reach with one arm across their body to help them roll onto their side. Place one hand on their shoulder and the other on their hip to help roll them. If the bed has a bed rail, they can use it to hold on to. The patient should be positioned on one side of the bed.
- Loosen the bed sheets from the empty half of the bed. Roll them up towards the center of the bed, toward the patient’s back. Half the mattress should now be exposed.
 Have patient bend knees and reach across body with arm to turn on side (can use guard rails if available). Roll up dirty sheet on one side towards patient’s back. Tuck rolled portion of sheet under patient.
Have patient bend knees and reach across body with arm to turn on side (can use guard rails if available). Roll up dirty sheet on one side towards patient’s back. Tuck rolled portion of sheet under patient. - Take a new clean bed sheet. Tuck in the edge of the sheet under the mattress, and then spread the sheet out to cover up the exposed half the mattress. Roll the remaining half the sheet and let it lie in the center of the bed, next to the patient’s back.
 Use clean sheet to cover exposed part of the mattress. Spread it and tuck it under patient.
Use clean sheet to cover exposed part of the mattress. Spread it and tuck it under patient. - Have the patient roll back to the center on their back. They will briefly be on top of the rolled up dirty sheet and rolled up portion of the clean sheet.
- Have them bend their knees again and reach across the other side of their body to roll to the opposite side. They should now be lying on half of the clean sheet.
 Have patient turn to other side on to the clean sheet. Pull off dirty sheet, and spread out other half of clean sheet.
Have patient turn to other side on to the clean sheet. Pull off dirty sheet, and spread out other half of clean sheet. - Remove the dirty sheet from the bed.
- Roll out the remaining half of the clean sheet and tuck it in.
- Have the patient return back to center.
These same steps can be used for changing out a soiled bed pad.
Read less
Comfort Care Medication Kit
The hospice care team will provide you with a comfort care medication kit to keep at home, which will help manage symptoms in a timely manner. This kit contains small amounts of different medicines to treat symptoms that may occur toward the end of life.
Read more
Information about dosage, instructions for administering, and which symptoms the medications help to treat can be found both on this site and in your hospice binder, although call hospice before using any of the medications.
Hospice Comfort Care Medication Kit and Usage Instructions
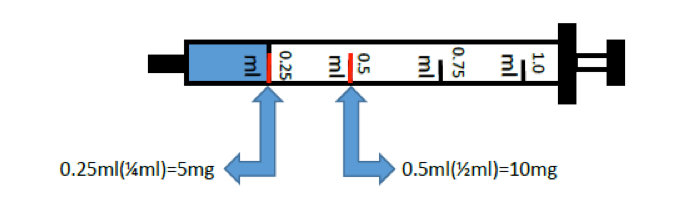
A one-millimeter syringe
| Medication | What It’s For | How to Take |
|---|---|---|
| Morphine Oral Solution
(see image above) |
A concentrated liquid medication used for pain and/or shortness of breath. Concentrated so only a small dosage is needed. A one-milliliter syringe (1.0 ml) without a needle (see image above) is included. | Can be swallowed or given under the tongue.
If swallowed, can be diluted in a small amount of fluid (water or juice) or given in soft food (pudding or applesauce) |
| Ativan tablet | Commonly used for anxiety, agitation, insomnia, seizures, and shortness of breath | May be swallowed or given under the tongue |
| Haldol oral solution | Commonly used for nausea, vomiting and/or agitation | May be swallowed or given under the tongue |
| Atropine solution | Commonly used for increased secretions
Note: Do not give in eye |
Given under the tongue |
| Phenobarbital tablets | Commonly used for agitation and/or seizures | May be swallowed or given rectally |
| Bisacodyl suppository | Commonly used for constipation. | Given rectally |
| Acetaminophen suppository | Commonly used for fever and/or mild pain | Given rectally |
| Lubricant | For ease of use for rectal administration of medications | For rectal use |
Please do not use any medication in the comfort care medication kit until instructed to do so by the hospice care team. If you have any questions regarding the comfort care medication kit, call the hospice care team, day or night.
Your hospice nurse will check your comfort kit regularly for expiration dates and to make sure you have the right medications with the correct quantity.
Read less
Constipation
Constipation or difficulty having a bowel movement is common for people with a serious illness. Cramps and pain associated with bowel movements may also be constipation.
Read more
Constipation can have several causes: not drinking enough water or fluids, slowing down of bodily functions, or as a side effect of some medications. Eating and drinking can be challenging for patients because of decreased appetite, energy level, and comfort when swallowing.
Simple ways to help with constipation
- Drink or sip small amounts of water throughout the day.
- Walk, move, or perform light activity.
- Ask if your hospice care team recommends a stool softener or mild laxative.
- Ensure privacy when using the bathroom. Some people may avoid having a bowel movement when others are around.
Talk with the hospice care team for recommendations that may make it easier to go to the bathroom.
Read less
Days and Hours Before Death – Signs and Symptoms
Some people want to know if they will be able to tell when the death of their loved one is near, while others prefer not to know. If you don’t want to know, we recommend you not read this section.
Read more
Please keep in mind that it is seldom possible to predict exactly when a person will die. However, knowing the common signs and symptoms your loved one could experience may help you feel better prepared.
Your loved one may experience some or all of these symptoms or ones not included on this list. If you have questions, please ask the hospice care team.
Breathing Patterns
As a person gets closer to death, breathing patterns may change. Sometimes there is:
- longer pauses between breaths, called apnea
- deep rapid breathing
- shallow rapid breathing
Confusion and Disorientation
Your loved one may see, hear, or experience things that you do not, like talking to someone who is not there. They may know they are approaching end of life. This is normal.
Confusion may be accompanied by agitation. Your loved one may
- move around in an agitated manner
- try to get out of bed, even when unsafe to do so
- cry or yell out
- speak nonsense
- pick at their clothes or bed sheets
For many people, it is often hard to see your loved one going through this process. Medications may help lessen these symptoms and keep the patient comfortable and safe.
Food and Liquids
It may provide some comfort to know that most people nearing death do not eat or drink, nor do they feel hunger. Our bodies no longer need or use nutrients as we near the end of life. Food and drinks do not taste good, and are often difficult to swallow or digest.
It can be hard for caregivers when their loved one does not want to eat or drink, but it’s a normal part of the dying process. Because of decreased input, and other physiological reasons, there will likely be a decrease in stool and urine output as well.
Fear of the Dying Process
Some may be afraid of not knowing what to expect as death nears, or they may fear a painful death. The hospice care team can help educate patients and families about pain and symptom management that may help to alleviate many of these perceived fears.
Fever
Some people have an elevated body temperature in the last days or hours of life. If your loved one is not awake or cannot swallow, there are rectal acetaminophen suppositories that can be used. There are also non-medication ways to reduce fever including, using a cool cloth on the patient’s forehead, behind their neck or in their groin area, a gentle fan can also help cool them down. Make sure that clothing or bedding is not heavy or confining.
Glazed Eyes
Many people do not see or track things well when they are nearing the end of life. Their eyes may appear glazed or may not close all the way.
Pre-Death Energy Surge
Some people experience a brief surge in energy in the hours or days before death. This may last from a few minutes to several hours. During this time, your loved one may talk more, be interested in engaging in conversation, or interested in eating or drinking. This may be a good time to be present with the loved one and enjoy the time together.
Secretions and Rattling Sound
Your loved one may have saliva or secretions that pool in the back of their throat and chest causing them to cough and even sound like they are choking. Although this may be frightening or disconcerting to witness, this does not mean your loved one is uncomfortable. Some people refer to this is the “death rattle.” There is a distinct gurgling, rattling sound that often happens to one’s breath in the hours and days prior to death. If this symptom becomes troublesome, ask the hospice care team about medication that may help with this. Again, this is a normal part of the dying process.
Sleep
Your loved one may sleep most, if not all, of the time. At some point, they may not wake easily. Hearing is usually the last sense to be lost. Continuing to speak to a loved one, telling them who you are and explaining what you are doing is both reassuring and calming.
Skin
Your loved one’s skin may be pale or clammy. When death is very imminent, or has just occurred, skin will be cool to the touch. The bottoms of the feet, palms of the hands, and area surrounding the mouth may be bluish in color.
Withdrawal
Your loved one may begin to lose interest in the world around them, and become withdrawn. They may speak less and have more time when they need to be quiet or need to sleep as they begin to transition from the outer world to their inner world. Gentle touch and presence can be a great reassurance.
It is common to have questions or concerns about symptoms. Please feel free to talk with the hospice care team.
What To Do When Your Loved One Is Actively Dying
Before death, people may think about whom they want with them when their loved one is dying. Some may want a close family member with them, others prefer a trusted spiritual leader, and some want to be alone with their loved one.
Many people like to softly hold their hand or lie next to their loved one as they face death. You may choose to gently speak to your loved one, or you may feel more comfortable sitting with them without speaking. Again, talk to the hospice care team if you have questions or concerns.
What To Do When Your Loved One Has Died
Once your loved one stops breathing for one minute or more, their heart will also stop.
- Call hospice immediately to let them know your loved one has died — you do not need to call 911.
- Call family members, or have someone make calls, to let people know your loved one has died. Collect phone numbers or email addresses beforehand and make sure your designated caller knows where this information is. The timing of doing this and how you do it is entirely up to you and what is best for you and your family.
- Call your chosen mortuary or funeral home. They will come to your home at a time you specify. Although you can keep your loved one’s body in your home for several hours, eventually they will need to be taken to be to a mortuary, crematorium, funeral home, or be donated to science. These arrangements need to be planned before death. A member of the hospice care team can tell you about services in your area and can assist you with this process.
For most people, decisions about what happens to one’s body after death can be difficult to make.
Some choose to donate their body to science to contribute to medical research and advancements.
For more information on the choice to donate, resources in your area, and support in talking to your family and friends about it, talk to your hospice social worker or click here for an overview on donating your body to science.
Read less
Dry Mouth and Lips
Patients on hospice often experience dry mouth and lips. This may be from long periods of resting with their mouth open or dehydration from not being able to drink or keep down enough fluid.
Read more
For dry lips
- Gently apply lip balm (like Chapstick®) or a layer of petroleum jelly (like Vaseline®). If the patient is using oxygen, use a non-petroleum based lip balm.
- For dried secretions on lips, use a warm, moist towel and gently dab to dampen them until they can be easily wiped away.
For dry mouth
- Offer frequent sips of water throughout the day, from a glass, a sippy cup, or a straw. Experiment to find what works best and is most comfortable.
- For those with difficulty swallowing, place a very small chip of ice in their mouth to melt on the tongue. Offer as needed, but make sure the ice chip is small enough to avoid choking.
- Try using oral mouth swabs (like Toothettes®), which are small sponges on a stick that can be moistened with water and gently placed inside the mouth. They can be found over the counter at drugstores. If you have difficulty finding them, ask the hospice care team.
Read less
Fall Prevention
Falling can be a serious problem, especially since hospice patients can be frail, weak, or dizzy. There are many things that caregivers and patients can do to reduce the chances of falling.
Read more
Organize the home to make it safer. Modify these common fall zones for safety:
Bedroom
- Keep a phone and a light within easy reach of the bed.
- Use a nightlight that automatically turns on when dark.
- It may help to use bed-risers or bed-rails to help patients more easily get in and out of bed.
Bathroom
- Install items to help patients stay stable, such as mounted grab bars in the shower and near the toilet.
- Place non-slip strips or plastic chairs in the shower.
- Avoid placing items deep or low in cabinets, and give patients liquid soap with a long-handled brush or bath mitts instead of bar soap. This keeps them from having to bend down too much.
- Automatic nightlights can be helpful.
Main living areas
- Keep cords bundled and out of the way, so no one will trip over them.
- Check rugs and carpets to make sure they don’t slip or have loose edges sticking up.
- Keep flashlights in multiple places that patient often accesses, like the kitchen counter or a side table in the living room.
- Avoid sitting on low chairs, couches, or beds, and keep a walking aid nearby for getting up.
Stairs
- Make sure there are sturdy arm rails on both sides of the steps spanning the entire length of the stairwell.
- Make sure the stairwell has good lighting and light switches are easy to find.
- Fix any loose or broken stairs.
- If the stairs have carpeting, make sure it is secure, or remove the carpeting and replace it with non-slip rubber treads.
In addition to caregivers organizing the home, patients can also take steps to avoid falls:
- Wear shoes with traction
- Avoid wearing long clothing, like long robes or pants with long hems, which can cause tripping.
- Make sure shoes are always tied, or switch to Velcro-fastened shoes.
Medical equipment can inadvertently lead to falls:
- Make sure wheelchairs are locked or walkers are stable before putting weight on them.
- Be careful with tubing, such as from an oxygen tank. It may be helpful to tape the tubing to the back of a patient’s shirt.
If a patient does fall, the patient should avoid trying to get up until they know they are all right. They should shout for help. Let the hospice care team know about the incident. This will help your team better understand how they are doing, what may have led to the fall, and prevent future falls from happening.
Read less
Help with Bathing
It is important that patients on hospice bathe regularly, for general cleanliness, infection prevention, and to feel comfortable. If the patient can get in and out of the bathtub or shower, you may only need to assist them or help them undress.
Read more
- If the patient has to step into the tub, have them sit on the edge of the tub, swing their legs over, and then stand. This will help prevent slipping. You can also put down non-slip mats or install grab bars. It may help to place a seat in the shower if it is difficult for the patient to stand.
- If the patient needs help bathing in the tub or shower, you can use a soft loofah or sponge to gently apply soap to parts of the body they cannot reach themselves. Make sure to use soap and shampoo that will not dry out the skin and rinse it off completely. Finish bathing by making sure the skin is gently but thoroughly dried.
- If the patient cannot get out of bed, they should still be bathed regularly. Start by filling a large bowl with warm water and placing it by the bed. Get several small towels – you’ll need one to clean the face and upper body, one for the lower body, and several towels for rinsing off soap and drying the skin. You only need to undress and clean one part of the body at a time.
- Start by gently wiping the area with a warm, wet towel. You can add a small amount of soap to the water and wipe the area again. After applying soap, make sure to rinse it all off by wiping the area again with a warm, wet towel that does not have soap on it. You may need to replace the water in the bowl several times during the wash. Pat dry the area gently and completely before moving to the next area.
- For face and hair, you may want to consider using a cream facial cleanser and dry shampoo. If a patient does not have the energy for bathing or a sponge bath, wiping skin gently with baby wipes is a good option.
Read less
Help with Using the Bathroom
Helping someone use the bathroom is an important responsibility. It can be challenging for both patients and caretakers alike. Whenever possible, help your loved one be as independent as possible for as long as possible. Always ask if they would like your assistance before trying to help.
Read more
If your loved one can get out of bed
- Ensure they get to the bathroom safely. Help with buttons, zippers, or removing articles of clothing if necessary.


- Some patients may need assistance while sitting on the toilet. Wrap your arm under their armpit and around their back to help lower them onto the toilet seat.
- After using the bathroom, they may need help cleaning themselves. Make sure you have washed your hands before helping. You may also find it helpful to wear a pair of plastic gloves.
- Start by wiping them with toilet paper, wiping from the front toward the back. Then use a wet wipe to finish cleaning them. Make sure they are clean and dry before putting their clothes back on.
- If the bathroom is located far away, ask the hospice care team for a commode (a small toilet on wheels that can be rolled near the bedside) or a wheelchair to help bring them to the bathroom. You may also want to place a chair halfway to the bathroom, so the patient can rest as they travel from the bedroom to the bathroom.
If your loved one cannot get out of bed or a chair
- Help them sit up if possible. Place lots of pillows behind them or, if they have an adjustable bed or chair, raise the back of it to sit them up. Men can use a handheld urinal provided by the hospice care team to urinate. For everything else, you can provide the patient with a bedpan, which is a portable toilet seat you can place on the bed under the patient to collect their waste.
- Make sure the bedpan is clean and kept nearby. You may have to help the patient place the bedpan underneath them. If possible, have the patient lift their bottom and back off the bed so you can slide it underneath them. You should support their back with one hand while you do this.
- If a patient cannot do this, have them roll to one side, helping them if needed. It can help to have them tuck their knees and hold on to a bed rail, if there is one. While the patient is on their side, place the bedpan on the bed by their bottom. Help the patient roll back, so the pan is positioned under their bottom. Help them with buttons, zippers and clothing that’s in the way.
- It is not uncommon for a patient to miss the bedpan or for some waste to spill out when you remove the bedpan. It’s helpful to place a waterproof pad underneath the bedpan to protect the bed. The hospice care team can provide these pads. If urine or stool spills on the sheets, change the sheets right away.
Try to give someone urinating or having a bowel movement as much privacy as possible. You can place a towel or sheet over them while they use the bathroom. It also helps to leave the room or create a calming routine, such as putting on soft music. After helping someone use the bathroom, make sure both of you wash your hands using soap and water or a hand sanitizer.
Read less
Help with Dressing
- Let patients dress themselves as much as possible. Some patients may simplify they type of clothing that they wear to dressing themselves, meaning they may not want to wear a bra or a shirt with lots of buttons. Loose-fitting clothing with elastic bands or front zippers are often easier to manage.
Read more
- If a patient does need help dressing, remember to be gentle and respectful. Have the clothes already out, so they do not need to wait while they are undressed. Also, they may want a choice in what they wear. Let them tell you what they would like. Make it easier by laying out two outfits and letting them choose.
- Helping with dressing is easiest when the patient is sitting in an upright position. Undress and dress one part of the body at a time to help keep them warm and preserve their privacy. If the patient has a weaker side, put the weaker arm through a sleeve first, so that they can use the stronger arm to put their arm through the second sleeve. When helping take off a shirt, help them remove their stronger arm first.
- When helping someone dress the bottom half of their body, have them lie flat. To remove clothing from around their waist, have them press the bottom of their feet into the bed and lift their hips and lower back off the mattress. They can rest after you pull the clothing below the knees. If they are too weak to do this, help them roll to one side so you can pull down one side of their waistband. Then help them roll to the other side to pull down the opposite side.
- Finally, dress their feet. Bunch up the socks so that they can slip their toes right into the toe of the sock and then pull them up and over the feet. Put on shoes or slippers that fit easily and comfortably. Avoid putting on anything tight or difficult to move in.
Read less
Incontinence, or Loss of Bladder or Bowel Control
It is common for people on hospice to sometimes lose control of their bladder or bowel, and they can often feel embarrassed or ashamed of their incontinence.
Read more
There are many ways caregivers can help patients maintain comfort, safety, and dignity during these moments.
Sometimes patients will not eat or drink to avoid having to go to the bathroom. This can cause them to feel weak or dizzy. Do everything you can to give the patient privacy, such as covering them with a loose sheet, asking others to leave the room, and leaving plenty of time for helping. Listen to the patient’s concerns and try your best to communicate with them about their needs.
For patients who can still use a bedpan or urinal on their own, keeping one nearby can help them avoid an accident.
Many patients will be unable to use a bedpan quickly enough. These patients will benefit from the use of an incontinence pad (often called “chucks”) or incontinence briefs (adult diapers).
Caregivers should place pads under the patient’s hips and thighs, and change them as soon as they become wet. If the patient cannot lift his or her hips off the pad for the caregiver to slide it out, caregivers can change the pad similar to how one changes a bedsheet.
Here’s how
- Have the patient bend his or her knees, and turn to one side.
- Roll-up half of the used pad toward the patient’s back. Have the patient then turn to the other side, over the rolled-up half of the pad.
- This should allow you to roll-up the rest of the pad and throw it away.
- Remember to clean the area with wipes and gently pat dry the skin. This is important because damp or unclean skin may become infected.
- Place a clean pad under the patient the same way.
Another option for patients is to wear incontinence briefs or adult diapers. They should be changed quickly once wet. If the patient cannot easily take off the briefs themselves, caregivers can have patients turn to the side and undo one side of the diaper at a time. Clean the area with wipes and pat dry.
If patients have a bowel movement, the same methods work to keep patients and their beds clean and dry. However, caregivers should remove any excrement with toilet paper first before cleaning with wipes and patting dry. Sometimes excrement can get stuck on hair in this area. It can help to put a little shaving cream on the area first and then use a damp cloth or toilet paper to remove the excrement.
Read less
Medication Administering
Giving your loved one medication and keeping track of what has been given are two of the most important jobs you will have as a caregiver.
Read more
All medications for your loved one will be provided by the hospice care team. For over-the-counter medication, they will provide specific instructions.
The hospice doctor and nurse will create a plan detailing how much and how often to give medications, as well as go over how to give them.
Your job is to make sure you administer them exactly the way the plan indicates, and track each time you do. This ensures your loved one has the correct dose at the correct time, to help keep them comfortable and safe. Use this Medication Chart (download here) to assist you.
If your loved one has side effects from any medication, or the medications do not seem to be having the desired effect, tell your hospice nurse immediately.
While it may feel overwhelming, remember that the hospice care team is here to help. If you have questions or concerns about giving or tracking medication, contact the hospice nurse.
Medications can be given in several different ways and the hospice nurse can show you how best to give them.
- By mouth or orally: Most pills, tablets, and capsules can be swallowed with liquid. Some tablets can also be crushed and placed in soft food, like applesauce. But not all pills can safely be crushed, so ask the hospice nurse before you give medication this way.
- By syringe: Some medicines, such as morphine, must first be drawn into a syringe. Drops from a syringe can be placed under the patient’s tongue or inside their cheeks.
- By inhalation: oxygen, as well as other breathing treatments, are inhaled. This usually involves breathing in the medicine by wearing a facemask or tube over the mouth or nose.
- By applying to the skin or topically: many creams and gels are rubbed on to the skin. Always wash your hands and put on gloves before applying a cream medication. Other topical medications may be patches worn on the skin. Remember to apply patches as directed and to look for any skin irritation or rashes under or around them.
- If medications cannot be taken orally, contact the hospice care team to discuss alternatives, such as giving medication rectally.
Read less
Medication Tracking
Tracking medications with this Medication Chart (download here) helps caregivers and the hospice care team know exactly the care your loved one has received and helps the next caretaker or hospice care team member to pick up where you left off.
Read more
Medicine given in the right dosage amount at the right time is crucial to its effectiveness and can keep your loved one safe and comfortable. Because there may be multiple caregivers helping care for your loved one, it is critical to keep track of medications so that your loved one’s medication works effectively. Missing a medication dose, or receiving an incorrect dose may cause dangerous side effects and complications.
Here are some tips on how to best keep track of medication:
- Drug name: Write the name of the drug. Include both its common name and the chemical name on the bottle, like Tylenol (acetaminophen).
- Appearance: Write the color and form, like pink circular pill, clear injectable liquid, or white cream. Medications may appear different from one prescription to the next. Keeping track of what a medication looks like can reduce the chance of giving the wrong medicine.
- Amount given: Be as specific as possible. Instead of writing 1 pill, write 1 pill – 250 milligrams.
- Time: Write the time given and whether it was before or after 12:00 noon. Use AM or PM.
- Symptom relief: Record why the medication was given. Was it for pain, nausea, shortness of breath?
Read less
Nausea
It is common for a hospice patient to experience nausea or lose their appetite. There are several practical things to try, which may help a patient feel more comfortable.
Read more
- Drinking soft drinks or carbonated beverages, such as ginger ale
- Slowly eating small bites of bland food, such as crackers
- Following the “BRAT” diet: bananas, rice, applesauce, toast. These foods are easy for the stomach to digest
- Eat and drink foods or liquids containing ginger, like ginger tea or gingerroot capsules
- Replace fluids lost by vomiting with light broth, sips of a carbonated beverage, gelatin, or a popsicle
- Avoid foods with strong flavors, aromas, or spices that may trigger nausea
- Serve food at a moderate or cool temperature, as hot foods can be painful or upsetting to the stomach
- Get some fresh air, either by opening a window, turning on a fan, or going outside
If these steps do not help with nausea, it can also be treated with medication. Call your hospice care team to find out if medication is an option.
Read less
Oxygen Safety
The hospice care team may provide you or your loved one with oxygen to help you breathe better. Oxygen is very effective and easy to use. However, you must be extremely careful with your oxygen because it can cause a fire or even an explosion.
Read more
Follow these tips for safe oxygen usage:
- Never smoke while using oxygen.
This is the number one cause of fires that occur while using oxygen. Do not smoke or let anyone else smoke inside your home if you have an oxygen tank. - Keep the oxygen tank away from anything that may spark or light a fire.
Keep it away from radiators, stoves, water heaters, pilot lights, heaters, or electrical devices like a hair dryer, electric razor, or electric toys. Be extra careful in the kitchen and bathroom, where many of these electronic or heating items are located. - Avoid oil and grease.
Take care that oily or greasy liquids do not spill on or near the oxygen tank. Also, avoid having oily or greasy liquids on your face near the oxygen mask. - Be aware of tubing.
Oxygen tanks come with long lines of tubing so you can move around while keeping the oxygen in a safe spot. Be careful not to trip, and point out tubing to others, such as visiting family members or children, so they don’t trip. - Store oxygen safely in open-air space.
Do not put an oxygen tank inside a closet or chest. Make sure it is somewhere where air around it can move freely. Never store your oxygen tank under a bed, in a car, near flammable materials or under clothing, bedding, or other items. Never have your cylinders standing upright without a tank stand. Your cylinders should be secured in a storage rack or stand or lying down. This prevents oxygen from building up in a single spot, which can cause a fire or explosion.
Read less
Pain Management
Helping a patient manage their pain is one of the main focuses of hospice care. The hospice care nurse will ask you about pain each time they see you. Based on your pain, they can provide and refill medications and suggest ways to help you be more comfortable.
Read more
Follow the pain management plan the hospice care team recommends. It may include over-the-counter pain medications (like ibuprofen or acetaminophen), other medications, or stronger drugs, such as opioids. Keep track of each medication, its name, the dosage, and the time given. It is very important that medication instructions are carefully followed.
Sometimes pain medications have side effects, such as sleepiness, nausea, or constipation. If you notice these side effects, tell the hospice care team. They can provide medications to ease these symptoms.
Here are some ways to manage pain in addition to medication:
- Relieve muscle soreness with hot and cold compresses.
- Relieve muscle stiffness with a warm shower or bath, or with a heating pad set on low over the area for 10-15 minutes. Make sure to not fall asleep with a heating pad on as it can result in burns or fire.
- Help the patient move to more comfortable positions.
- Gently massage tight or cramped muscles.
- Alternative therapies that distract from pain, like meditation, breathing exercises and our free guided imagery can be beneficial in helping you or your loved one cope. Aromatherapy (scented plant oils) may help also help with relaxation.
If you feel you are having trouble controlling your or your loved one’s pain, please call the hospice care team.
Read less
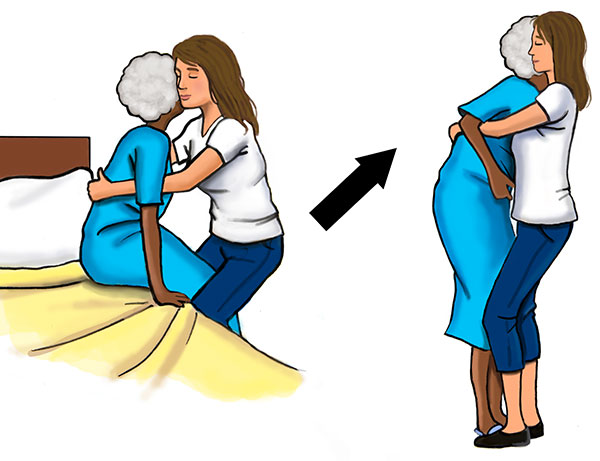
Safe Lifting Techniques
As a caregiver, it is important to be mindful of how you lift your loved one so that it is safe for both them and you.
Read more
Patients will often need help repositioning themselves in bed. Repositioning a patient frequently can help prevent bedsores and enhance their comfort. However, it’s important to move a patient safely to keep oneself and the patient from getting injured. If possible, always raise the bed up to a height that allows you to keep your back straight when moving a patient.
To turn them on their side
Pull any blankets or sheets down to the foot of the bed. Put up the bedrails if the bed has them. If not, stand to the side of the bed you want the patient to turn to. With the patient lying on their back, have the patient bend their knees so the bottom of their feet are flat on the bed. Next, have the patient reach one arm across their body and hold on to the bed rail that they want to turn toward. If there is no bed rail, they can hold your hand. Using the bed rail or your hand for support, the patient should twist and pull themselves onto their side. Replace the sheets over them and position the pillow, so it is supporting their head. You can also place a pillow firmly behind their back and hips to help keep them from rolling back.

To slide them up in bed
Sometimes patients that are sitting up in bed slide down towards the foot of the bed and need help to slide back up. To do this, first check to see that there is a towel or sheet positioned behind their neck and back, with some sticking out on either side of them. Next, lower the head of the bed down so the entire mattress is flat and the patient is on his or her back. Pull any blankets or sheets down to the foot of the bed. Have the patient bend their knees and press the bottoms of their feet into the mattress. If there are 2 people available, have one stand at either side of the patient. Hold the towel underneath them, gripping the part near the neck and shoulders, and count to three. On three, have the patient press with their feet while you lift them slightly with the towel and slide them toward the head of the bed.

If only one person is available, slide one arm under the neck and shoulders and the other under the thighs. On the count of three, have the patient press with their feet while you lift them slightly and slide them toward the head of the bed. Reposition their pillow and cover them again with the sheets.

Read less
Shortness of Breath
People who have a serious illness may experience shortness of breath, which can feel like tightness in the chest or a sensation of breathing hard while just walking or even resting. A person experiencing shortness of breath may need to take several quick, short breaths or may have difficulty talking, especially while physically moving. Some patients with shortness of breath may not be getting enough oxygen. If you suspect this may be true for you or your loved one, please let your hospice care team know as soon as possible.
Read more
Since shortness of breath can cause anxiety for patients and caregivers, here are several helpful treatments for patients:
- Oxygen and/or direct breathing of room air: a patient wears a small tube or mask on their face that provides oxygen or room air through their nose or mouth while they breathe. The hospice care team can instruct you on how to use the mask, as well as how to manage oxygen safely.
- Medicated breathing treatments: a patient wears a small mask over their mouth and nose that is connected to a pump that turns medicine into a mist, which the patient breathes in for 10 to 20 minutes. This treatment can help open up the lungs to make breathing easier.
- Morphine: Morphine and related medications can help a patient breathe more deeply and slowly. When taking morphine, make sure to follow instructions from the hospice care team so it is used safely and effectively. Depending on its form, it may be taken as a pill or with a dropper under their tongue. Keep track carefully of the dose and time of each use.
Other suggestions
- Cool the room and open the drapes or blinds, so the room feels open and airy, and not small and confined. If possible, open windows to let in a breeze or place a fan to gently blow on the patient’s face if they are comfortable with it.
- Use a cool mist vaporizer to help keep the room air from getting too dry.
- Help the patient with anxiety or worry by doing meditation, guided imagery exercises, or simply by being there to provide companionship. Being less anxious and more relaxed may help slow breathing and lessen feelings of stress that comes from experiencing shortness of breath.
Read less